When it comes to dialysis treatment, it’s important that you choose the method right for you. As dialysis can be such a time-consuming process, many people choose to do their haemodialysis at home instead of in a centre. Home haemodialysis offers flexibility, allowing you to organise your sessions around your lifestyle rather than scheduling at a satellite or hospital dialysis unit.
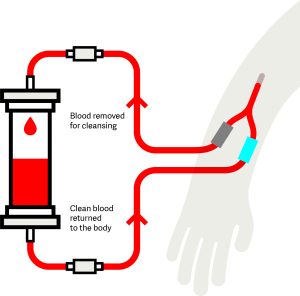
Doing your haemodialysis at home follows the same process as centre-based haemodialysis, except that it’s done at home. Haemodialysis requires vascular access, which is a way to reach your blood through a fistula, graft or haemodialysiss catheter. You’ll need to place a needle into your vascular access to allow the blood to flow from your body through tubes to the dialysis machine. Blood is cleaned through a special filter, called a dialyser, before returning to your body.
With the right planning and education, you will have the option of setting up haemodialysis in your home. Your home will need to have access to electricity, a water supply, and room to set up the supplies and equipment.
Equipment is provided to your home free of charge, however, you still need to take into consideration the initial costs like installing a new plumbing set up, and ongoing costs such as increased water and electricity bills. You may be eligible for financial support from the government.
If you choose home-based haemodialysis, you’ll need to be able to insert your own needles, which are used to extract your blood and clean it through the dialysis machine. Training takes about six to eight weeks, and you’ll have to travel to your closest dialysis centre.
Not everyone’s home is suitable for haemodialysis, so if you’re considering it, you should learn as much as you can. Our ‘Introduction to…’ series featuring home haemodialysis is a great place to start.
As mentioned, undergoing your haemodialysis at home can offer you greater flexibility. You’ll need to undergo this type of dialysis at least three times a week, with each session lasting four to five hours. You can also do it overnight while you sleep, which can be more comfortable to do in your own home.
Many people alternate their haemodialysis treatment every second day, equalling a total of four sessions a week.
Choosing home haemodialysis offers flexibility for your life and schedule, but it’s not the only home-based dialysis treatment. Peritoneal dialysis is another alternative to home haemodialysis. Learn more about your dialysis options in the home.
Additional resources

An Introduction to Home Dialysis

An Introduction to Kidney Disease Treatment Options

An Introduction to Haemodialysis
Last updated: October 2025


