Understanding Peritoneal Dialysis for Kidney Failure
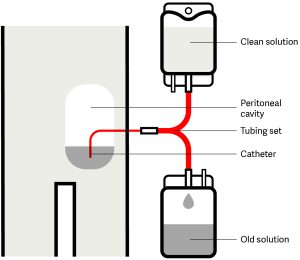
Peritoneal dialysis is a treatment option for kidney failure. After being trained by your healthcare team, you can undergo this method at home, providing you with additional comfort during your treatments.
There are two different types of peritoneal dialysis – Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD), to suit different lifestyles and preferences